-
PDF
- Split View
-
Views
-
Cite
Cite
Niek Koenders, Sandra Potkamp-Kloppers, Yvonne Geurts, Reinier Akkermans, Maria W G Nijhuis-van der Sanden, Thomas J Hoogeboom, Ban Bedcentricity: A Multifaceted Innovation to Reduce Sedentary Behavior of Patients During the Hospital Stay, Physical Therapy, Volume 101, Issue 7, July 2021, pzab054, https://doi.org/10.1093/ptj/pzab054
Close - Share Icon Share
Abstract
The purpose of this study was to explore differences in sedentary behavior, length of hospital stay, and discharge destination of patients before and after the Ban Bedcentricity implementation at ward level.
The Ban Bedcentricity innovation and implementation procedure were implemented at the cardiothoracic surgery, cardiology, and orthopedics-traumatology wards. Sedentary behavior data were collected 2 weeks before and after the implementation using behavioral observations and analyzed with Pearson chi-square. Length of hospital stay and discharge destination data were collected from all admitted patients and analyzed with multiple and logistic regression analyses.
Behavioral observations showed that in 52% of the observations, patients were lying in bed before implementation and 40% after implementation at the cardiothoracic surgery, 64% and 46% at the cardiology, and 53% and 57% at the orthopedics-traumatology wards, respectively. The mean length of hospital stay after implementation (compared with implementation before) was 5.1 days at the cardiothoracic surgery (n = 1923; mean = +0.13 days, 95% CI = −0.32 to 0.60), 2.6 days at the cardiology (n = 2646; mean = −0.22 days, 95% CI = −0.29 to −0.14), and 2.4 days at the orthopedics-traumatology wards (n = 1598; mean = +0.28 days, 95% CI = 0.06 to 0.50). After the implementation, more patients were discharged home from the cardiothoracic surgery (odds ratio [OR = 1.23], 95% CI = 1.07 to 1.37) and cardiology wards (OR = 1.37, 95% CI = 1.22 to 1.49), and no statistically significant difference was found at the orthopedics-traumatology ward (OR = 1.09, 95% CI = 0.88 to 1.27).
The results indicate beneficial outcomes after the implementation with less sedentary behavior and proportionately more patients being discharged home compared with before the implementation. However, little information is available about the adoption and fidelity of Ban Bedcentricity; therefore, outcomes should be interpreted with caution.
This multifaceted innovation to reduce sedentary behavior of patients during the hospital stay seems to be promising, with outcomes indicating less sedentary behavior in patients and more patients being discharged home after the implementation.
We introduced Ban Bedcentricity, an intervention to reduce the amount of time patients lie in the hospital bed during their hospitalization. This study shows that after the introduction of Ban Bedcentricity, patients lie in bed less and are more often discharged home.
Introduction
The hospital bed plays an important role in hospital care. For example, single-bed or multi-bed rooms serve as a starting point for hospital architecture.1 The logistics of a hospital are dependent on the arrangement of beds,2 and the ability of a hospital to care for patients is commonly expressed in bed occupancy.3 The bed is a culturally accepted place where patients can be cared for while promoting recovery and well-being.4 However, the hospital bed can also elicit physical inactivity because it implies that patients are ill and need to lie in bed.5
Sedentary behavior, especially lying in bed during daytime, is very common in patients during the hospital stay.6–9 Well-known adverse outcomes of excessive sedentary behavior are, among others, a prolonged hospital stay and institutionalization as a consequence of functional decline.9,10 Adverse outcomes can be prevented or cured by reducing sedentary behavior and improving physical activity.11 To reduce sedentary behavior, we have developed and implemented the multifaceted innovation called Ban Bedcentricity. In summary, Ban Bedcentricity aims to (1) improve the mindset and knowledge and attitude of patients, close relatives, and health care professionals regarding the benefits of physical activity and risks of sedentary behavior for patients; (2) provide adequate materials to support inpatient physical activity; and (3) optimize the hospital cultural environment to elicit physical activity of patients.
However, it is unknown whether Ban Bedcentricity contributes to less sedentary behavior and better outcomes. Therefore, the current study aims to explore differences in sedentary behavior, length of hospital stay, and discharge destination before and after the implementation of Ban Bedcentricity at ward level.
Methods
Study Design
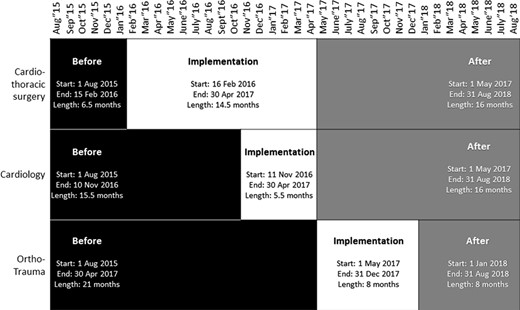
The current study used a before-after design to evaluate outcomes of the Ban Bedcentricity innovation at the Radboud University Medical Center, Nijmegen, the Netherlands.12,13 This explorative study used prospectively collected behavioral observations data to analyze before-after differences in sedentary behavior and physical activity of patients at ward level. In addition, routinely collected, standardized data were used to analyze before-after differences in length of hospital stay and discharge destination at ward level. The Ban Bedcentricity implementation procedure was performed at the cardiothoracic surgery ward between February 16, 2016, and April 28, 2017; at the cardiology ward between November 11, 2016, and April 28, 2017; and at the orthopedics-traumatology ward between May 1, 2017, and December 29, 2017 (Fig. 1). Study reporting followed the Strengthening the Reporting of Observational Studies guideline14 and Reporting of Studies Conducted Using Observational Routinely Collected Data statement.15 Ethical approval was granted by the local Ethics Committee (registration number 2018–4172) of the Radboudumc, Nijmegen, the Netherlands.
The Ban Bedcentricity implementation procedure started in the implementation phase. This figure shows the different study phases for each hospital ward: before implementation (black), in the implementation phase (white), and after implementation (grey). The implementation activities started at the cardiothoracic surgery ward on February 16, 2016, the cardiology ward on November 11, 2016, and the orthopedics-traumatology (ortho-trauma) ward on May 1, 2017.
Project Team
Two physical therapists (Y.G. and S.B.) managed the project team. They coordinated the implementation of Ban Bedcentricity at the different hospital wards, and they were the first contact persons for the managers of the hospital wards. The project team consisted of implementation, research, and advisory officers. One implementation officer (H.R. or D.M.) performed all implementation activities in collaboration with the multidisciplinary care team of the hospital ward (physical therapists, nurses, and physicians/surgeons). The implementation officer acted as the first contact person for all patients, close relatives, and health care professionals. The research officers managed the evidence base, practical evaluations, and scientific reporting. The advisory officers gave solicited and unsolicited advice and included members of the board of directors, patient advisory board, department of construction, department of finances, Radboudumc REshape Center for Innovation, and the iBoard.
The Ban Bedcentricity Innovation
The Ban Bedcentricity innovation aimed to reduce sedentary behavior in patients during the hospital stay by cultural change. The Ban Bedcentricity implementation activities were performed at 3 different hospital wards and focused on improving the mindset of patients, close relatives, and health care professionals to reduce sedentary behavior and stimulate physical activity. Moreover, (new) materials were developed and provided to patients, and the hospital design and construction were changed. Before implementation, potential innovations in mindset, materials, and hospital environment were discussed. Actual implementation activities were chosen and developed in co-creation with patients, health care professionals, implementation officers, and project managers in the implementation phase. In the phase “after implementation” of Ban Bedcentricity, all implementation activities were completed.
Mindset
The implementation officers updated all the digital and off-line patient-related information material in cooperation with the communication department to inform patients about the risks of sedentary behavior and the benefits of physical activity. All patients received the patient information folder at their time of hospitalization with information about the importance of physical activity and details of Ban Bedcentricity. In addition, all patients with an email account received the patient information folder digitally. Posters that summarized the Ban Bedcentricity patient information were attached to the walls of all patient rooms. The implementation officers also updated all information material for health care professionals and constructed an online website to provide all relevant information about the Ban Bedcentricity innovation. All health care professionals received the health care professional information folder by email. In addition, posters that summarized the Ban Bedcentricity professional information were attached to the walls of all lunch areas. The implementation officers performed frequent (25 times, 4 hours each) coaching on the job sessions for health care professionals. Between 5 and 7 health care professionals were coached every 4 hours. Twenty-five on-the-job coaching sessions were planned on different working days and time slots (ie, mornings and afternoons), with the aim of coaching different health care professionals working in different team compositions. Ideas, insights, practical tips, and advice regarding sedentary behavior or physical activity of patients were discussed 3 times a week in short educational sessions after lunch.
Materials
The implementation officers provided relax chairs, a bed cover, and carry-on walkers with intravenous systems for patients to encourage sitting and walking of patients during the hospital stay (Suppl. Material, Figs. S1a and S1b). They also provided e-health solutions for patients to access exercise programs and stimulate physical activity (Suppl. Material, Fig. S1c).
Hospital Environment
Changes in the hospital environment were chosen and developed in co-creation in the implementation phase. For example, patients mentioned that they needed handrails to feel safe while walking. The type of handrail was determined with test material in consultation with patients, health care professionals, implementation officers, and the project managers. In addition, implementation officers introduced new e-Health technologies to match the needs of patients and health care professionals. Furthermore, the health care professionals indicated where they liked to have the movement and relaxation area and how it should be arranged. All changes in the hospital environment were implemented in all 3 hospital wards. The employees of the construction department designed and installed the new hospital environment (Suppl. Material, Figs. S2a, S2b, and S2c). All patients and health care professionals were informed about the new hospital environment with the information folders and posters. In addition, instructions were given during the on-the-job coaching sessions and educational sessions by the implementation officers. Questions were answered, and tests with the new e-Health technologies were carried out by the project managers on joint walking tours with health care professionals who had additional questions.
The Ban Bedcentricity Implementation Procedure
Table 1 shows the implementation manual with details of the implementation procedure. The implementation procedure followed 3 steps to introduce the Ban Bedcentricity innovation at the hospital ward: orientation, action, and finalization. The main purpose of the orientation phase was to meet the managing staff, confirm the ambition to implement Ban Bedcentricity, and to sign the project budget. Then, the action phase started with a kick-off meeting to involve all stakeholders (ie, nurses, allied health care professionals, medical staff, and managing staff), followed by all implementation activities as described in the Ban Bedcentricity implementation manual. The finalization phase started when all the selected implementation activities were performed, including the availability of materials and the change of the hospital ward design and construction. Part of the finalization was the installation of a Ban Bedcentricity Champion for long-term follow-up. The implementation activities were tailored to the needs and preferences of the hospital ward staff. For example, the content of information material and the supply of additional materials (eg, exercise kits, home trainer, sit-to-stand assist) were tailored to the specific patient population at that hospital ward. The design and reconstruction activities at the cardiothoracic surgery ward required an additional 10 weeks more than planned due to a delay in the design and reconstruction of the hospital ward.
Details of the Implementation Procedure of the Ban Bedcentricity Innovationa
| . | Frequency . | Time . | In Charge . |
|---|---|---|---|
| Orientation | |||
| Meet with managing staff | 1 | 60 min | PM |
| Secure Ban Bedcentricity in mission statement | 1 | n.a. | IO |
| Draw and sign project budget and planning | 1 | n.a. | PM |
| Action | |||
| Kick-off meeting with nurses, allied health care professionals, medical staff, and managing staff (and volunteers) | 1 | 30 min | PM |
| Appoint a Ban Bedcentricity Champion | 1 | n.a. | PM |
| Perform participative observations | 25 | 4 h | IO |
| Lead educational sessions for health care professionals | >25 | 30 min | IO |
| Develop information material | 1 | n.a. | IO |
| Screen materials | 1 | n.a. | IO |
| Introduce new materials, eg, relax chairs and clothes | 1 | >3 mo | IO |
| Renovate design and reconstruction of hospital ward | 1 | >3 mo | PM |
| Finalization | |||
| Install Ban Bedcentricity Champion | 1 | n.a. | PM |
| Deliver certificate of excellence | 1 | n.a. | PM |
| Provide closing report | 1 | n.a. | PM |
| . | Frequency . | Time . | In Charge . |
|---|---|---|---|
| Orientation | |||
| Meet with managing staff | 1 | 60 min | PM |
| Secure Ban Bedcentricity in mission statement | 1 | n.a. | IO |
| Draw and sign project budget and planning | 1 | n.a. | PM |
| Action | |||
| Kick-off meeting with nurses, allied health care professionals, medical staff, and managing staff (and volunteers) | 1 | 30 min | PM |
| Appoint a Ban Bedcentricity Champion | 1 | n.a. | PM |
| Perform participative observations | 25 | 4 h | IO |
| Lead educational sessions for health care professionals | >25 | 30 min | IO |
| Develop information material | 1 | n.a. | IO |
| Screen materials | 1 | n.a. | IO |
| Introduce new materials, eg, relax chairs and clothes | 1 | >3 mo | IO |
| Renovate design and reconstruction of hospital ward | 1 | >3 mo | PM |
| Finalization | |||
| Install Ban Bedcentricity Champion | 1 | n.a. | PM |
| Deliver certificate of excellence | 1 | n.a. | PM |
| Provide closing report | 1 | n.a. | PM |
aIO = implementation officer; n.a. = not applicable; PM = project manager; RO = research officer.
Details of the Implementation Procedure of the Ban Bedcentricity Innovationa
| . | Frequency . | Time . | In Charge . |
|---|---|---|---|
| Orientation | |||
| Meet with managing staff | 1 | 60 min | PM |
| Secure Ban Bedcentricity in mission statement | 1 | n.a. | IO |
| Draw and sign project budget and planning | 1 | n.a. | PM |
| Action | |||
| Kick-off meeting with nurses, allied health care professionals, medical staff, and managing staff (and volunteers) | 1 | 30 min | PM |
| Appoint a Ban Bedcentricity Champion | 1 | n.a. | PM |
| Perform participative observations | 25 | 4 h | IO |
| Lead educational sessions for health care professionals | >25 | 30 min | IO |
| Develop information material | 1 | n.a. | IO |
| Screen materials | 1 | n.a. | IO |
| Introduce new materials, eg, relax chairs and clothes | 1 | >3 mo | IO |
| Renovate design and reconstruction of hospital ward | 1 | >3 mo | PM |
| Finalization | |||
| Install Ban Bedcentricity Champion | 1 | n.a. | PM |
| Deliver certificate of excellence | 1 | n.a. | PM |
| Provide closing report | 1 | n.a. | PM |
| . | Frequency . | Time . | In Charge . |
|---|---|---|---|
| Orientation | |||
| Meet with managing staff | 1 | 60 min | PM |
| Secure Ban Bedcentricity in mission statement | 1 | n.a. | IO |
| Draw and sign project budget and planning | 1 | n.a. | PM |
| Action | |||
| Kick-off meeting with nurses, allied health care professionals, medical staff, and managing staff (and volunteers) | 1 | 30 min | PM |
| Appoint a Ban Bedcentricity Champion | 1 | n.a. | PM |
| Perform participative observations | 25 | 4 h | IO |
| Lead educational sessions for health care professionals | >25 | 30 min | IO |
| Develop information material | 1 | n.a. | IO |
| Screen materials | 1 | n.a. | IO |
| Introduce new materials, eg, relax chairs and clothes | 1 | >3 mo | IO |
| Renovate design and reconstruction of hospital ward | 1 | >3 mo | PM |
| Finalization | |||
| Install Ban Bedcentricity Champion | 1 | n.a. | PM |
| Deliver certificate of excellence | 1 | n.a. | PM |
| Provide closing report | 1 | n.a. | PM |
aIO = implementation officer; n.a. = not applicable; PM = project manager; RO = research officer.
Study Population
The study population used for comparison in the data analysis included patients after open heart surgery at the cardiothoracic surgery ward before implementation (August 1, 2015–February 15, 2016), in the implementation phase (February 16, 2016–April 30, 2017), and after implementation (May 1, 2017–August 31, 2018); myocardial infarction or heart failure at the cardiology ward before implementation (August 1, 2015–November 10, 2016), in the implementation phase (November 11, 2016–April 30, 2017), and after implementation (May 1, 2017–August 31, 2018); and elective joint replacement or traumatic fracture surgery at the orthopedics-traumatology ward before implementation (August 1, 2015–April 30, 2017), in the implementation phase (May 1, 2017–December 31, 2017), and after implementation (January 1, 2018–August 31, 2018) (Figure). Patients with a hospital stay less than 6 hours were excluded, because this group included only patients with routine follow-up after surgery without an actual admission to the hospital ward.
Data Collection and Outcomes
Data on the sedentary behavior and physical activity of patients were collected using behavioral observations during the 2 weeks in the “before implementation” phase and 2 weeks in the “after implementation” phase. The observations were performed at the cardiothoracic surgery ward in December 2015 (before implementation) and December 2017 (after implementation), in the cardiology ward in October 2016 (before) and May 2017 (after), and in the orthopedics-traumatology ward in March 2017 (before) and April 2018 (after). Each of the 3 wards was observed over 2 consecutive weeks on weekdays between 8 am and 4 pm.16 The observers walked around the ward every 3 minutes, and each patient at the ward was observed for about 10 seconds during each 3-minute interval. This procedure was repeated 10 times in a row by 1 observer. As a result, each observation included data of 30 minutes. Ten observations of 30 minutes each added to a total of 5 hours data for each ward before implementation and 5 hours data after implementation. The timing of observations was block-randomized by ward: 5 between 8 am and 12 pm, and 5 between 12 pm and 4 pm. All observations were performed in a different 30-minute time slot so there was no overlap. The route through the ward was standardized throughout each observation. The posture of patients was noted at a standardized case report form as lying in bed with back rest, sitting on (the edge of) a bed, sitting on a chair, standing, walking, or posture unknown. The observer anonymously noted the observed posture and did not note patient characteristics or time spent lying, sitting, standing, or walking. If a patient moved at the time of observation from 1 posture to another (eg, lying to sitting), the end posture was reported (eg, sitting). If a patient room was closed, the observers scored “unknown.” Patients were not followed off the ward or intruded on if behind closed doors. Behavioral observation methods similar to these showed reasonable agreement with actual sedentary behavior of patients during their hospital stay.17
Data on the length of hospital stay and discharge destination were collected from patients at the 3 hospital wards between August 1, 2015, and August 31, 2018. This study used standardized data extraction syntax, constructed by the business intelligence and analytics department to ensure anonymous and independent data extraction from electronic patient records. Patient characteristics (age, sex), surgery (yes or no), and physical therapy treatment (yes or no) were extracted and used to build an adjusted model. The hypothesis was that the presence of a physical therapist during the hospital stay, even if this was a single contact, might have an impact on the length of hospital stay and discharge destination. Length of hospital stay was measured in days (2 decimals) between hospital admission and discharge. Discharge destination was dichotomized as patients discharged home or discharged to another destination than home. More detailed information, for example on discharge to a rehabilitation center or nursing home, could not be retrieved from the electronic health records.
Data Analysis
Data were analyzed using SPSS statistics 22.0 for Windows.18 Descriptive statistics were used to summarize data on all relevant patient characteristics. Pearson chi-square was used to test differences in observations of patients lying, sitting, or standing/walking between before and after the implementation at ward level. Medians and interquartile ranges were calculated for the length of hospital stay, and percentages and odds ratios (OR) were calculated for patients being discharged home. The skewed length of hospital stay data were first log-transformed and then analyzed with a linear regression model. Length of hospital stay outcomes were presented as absolute and relative differences between study phases with 95% CI, with the “before implementation” phase as reference. Logistic regression analysis was performed to test differences between the study phases in patients being discharged home. The outcomes were expressed in OR with 95% CI, whereas an OR higher than 1 indicated that more patients were being discharged home. An OR of being discharged home of 1.10 after implementation should be interpreted as an increase of 10% in the odds of patients being discharged home compared with before the implementation. Multivariate linear and logistic regression analysis were used to construct an adjusted model with the study phases as a factor and age, sex, surgery, and physical therapy treatment as covariates. A 2-sided P < .05 was considered statistically significant.
Three a priori decisions were made regarding the data analysis: (1) the decision for a specific start and end point of the study, (2) the decision to not adjust for seasonality, and (3) the decision not to include prior living situation as a covariate. Therefore, we performed 3 sensitivity analyses to test the robustness of the length of hospital stay and discharge destination outcomes and to assess to what extent the decisions impacted our outcomes. Differences in statistical significance (eg, changes from P < .05 to P ≥ .05) and differences in direction of outcomes (eg, changes from more patients being discharged home to less patients being discharged home) between the outcomes of the primary analyses and sensitivity analyses were discussed. The first a priori decision was to use August 1, 2015, as the starting point and August 31, 2018, as the end point of this study. In the first sensitivity analysis, data of patients in the first month (August 1, 2015–August 31, 2015) and/or last month (August 1, 2018–August 31, 2018) were excluded to check for differences in outcomes with other study start or endpoints. The second a priori decision was to use all available data without considering seasonal influences. The second sensitivity analysis included only data of patients at the cardiothoracic surgery ward between July and January, cardiology ward between December and April, and orthopedics-traumatology ward between March and August. The third a priori decision was not to include prior living situation as a covariate in the adjusted model. In the third sensitivity analysis, we added prior living situation data. Prior living situation was extracted with the standardized data extraction syntax and dichotomized as “admitted from home” or “not admitted from home.”
Results
Sedentary Behavior and Physical Activity
Table 2 shows the differences in proportion of observations in patients lying, sitting, standing, and walking between before and after the implementation at ward level. In total, 30 hours of sedentary behavior and physical activity data were collected. Before the implementation at the cardiothoracic surgery ward, there were 52% of the observations of patients lying in bed, 42% sitting, and 6% standing/walking. After the implementation, the distribution of observations changed statistically significantly (P = .02) to 40% lying in bed, 47% sitting, and 13% standing/walking. Before the implementation at the cardiology ward, 64% of the observations were patients lying in bed, 28% sitting, and 8% standing/walking. After the implementation, the distribution of observations changed statistically significantly (P < .01) to 46% lying in bed, 44% sitting, and 10% standing/walking. Before the implementation at the orthopedics-traumatology ward, 53% of the observations were of patients lying in bed, 42% sitting, and 5% standing/walking. After the implementation, there was no statistically significant difference (P = .47) in the distribution of observations of patients lying in bed (57%), sitting (37%), and standing/walking (6%).
Differences in Sedentary Behavior of Patients Before and After Implementation at Ward Level, Statistically Tested With Pearson Chi-Squarea
| . | Before, n/N . | % . | After, n/N . | % . | P . |
|---|---|---|---|---|---|
| Cardiothoracic surgery ward | |||||
| Lying | 81/156 | 52% | 76/191 | 40% | .02 |
| Sitting | 66/156 | 42% | 90/191 | 47% | |
| Standing/walking | 9/156 | 6% | 25/191 | 13% | |
| Cardiology ward | |||||
| Lying | 78/122 | 64% | 77/167 | 46% | <.01 |
| Sitting | 34/122 | 28% | 73/167 | 44% | |
| Standing/walking | 10/122 | 8% | 17/167 | 10% | |
| Orthopedics-traumatology ward | |||||
| Lying | 138/260 | 53% | 180/316 | 57% | .47 |
| Sitting | 109/260 | 42% | 117/316 | 37% | |
| Standing/walking | 13/260 | 5% | 19/316 | 6% | |
| . | Before, n/N . | % . | After, n/N . | % . | P . |
|---|---|---|---|---|---|
| Cardiothoracic surgery ward | |||||
| Lying | 81/156 | 52% | 76/191 | 40% | .02 |
| Sitting | 66/156 | 42% | 90/191 | 47% | |
| Standing/walking | 9/156 | 6% | 25/191 | 13% | |
| Cardiology ward | |||||
| Lying | 78/122 | 64% | 77/167 | 46% | <.01 |
| Sitting | 34/122 | 28% | 73/167 | 44% | |
| Standing/walking | 10/122 | 8% | 17/167 | 10% | |
| Orthopedics-traumatology ward | |||||
| Lying | 138/260 | 53% | 180/316 | 57% | .47 |
| Sitting | 109/260 | 42% | 117/316 | 37% | |
| Standing/walking | 13/260 | 5% | 19/316 | 6% | |
Differences in Sedentary Behavior of Patients Before and After Implementation at Ward Level, Statistically Tested With Pearson Chi-Squarea
| . | Before, n/N . | % . | After, n/N . | % . | P . |
|---|---|---|---|---|---|
| Cardiothoracic surgery ward | |||||
| Lying | 81/156 | 52% | 76/191 | 40% | .02 |
| Sitting | 66/156 | 42% | 90/191 | 47% | |
| Standing/walking | 9/156 | 6% | 25/191 | 13% | |
| Cardiology ward | |||||
| Lying | 78/122 | 64% | 77/167 | 46% | <.01 |
| Sitting | 34/122 | 28% | 73/167 | 44% | |
| Standing/walking | 10/122 | 8% | 17/167 | 10% | |
| Orthopedics-traumatology ward | |||||
| Lying | 138/260 | 53% | 180/316 | 57% | .47 |
| Sitting | 109/260 | 42% | 117/316 | 37% | |
| Standing/walking | 13/260 | 5% | 19/316 | 6% | |
| . | Before, n/N . | % . | After, n/N . | % . | P . |
|---|---|---|---|---|---|
| Cardiothoracic surgery ward | |||||
| Lying | 81/156 | 52% | 76/191 | 40% | .02 |
| Sitting | 66/156 | 42% | 90/191 | 47% | |
| Standing/walking | 9/156 | 6% | 25/191 | 13% | |
| Cardiology ward | |||||
| Lying | 78/122 | 64% | 77/167 | 46% | <.01 |
| Sitting | 34/122 | 28% | 73/167 | 44% | |
| Standing/walking | 10/122 | 8% | 17/167 | 10% | |
| Orthopedics-traumatology ward | |||||
| Lying | 138/260 | 53% | 180/316 | 57% | .47 |
| Sitting | 109/260 | 42% | 117/316 | 37% | |
| Standing/walking | 13/260 | 5% | 19/316 | 6% | |
Length of Hospital Stay and Being Discharged Home
Table 3 shows the descriptive characteristics of the included patients. Data on the length of hospital stay and patients being discharged home were collected from 18,163 patients with a mean age of 59.1 years (SD = 17.9). The majority were male (57%) and underwent surgery (53%). Our database included 4544 patients admitted to the cardiothoracic surgery ward (mean age = 61.1 years, SD = 16.6); 6038 patients at the cardiology ward (mean age = 64.7 years, SD = 15.6), and 7581 at the orthopedics-traumatology ward (mean age = 53.4 years, SD = 18.7). The geometric mean length of hospital stay was 5.1 days (SD = 2.7) at the cardiothoracic surgery ward, 2.6 days (SD = 2.8) at the cardiology ward, and 2.3 days (SD = 3.2) at the orthopedics-traumatology ward. In total, 2592 patients (57%, 17 missing) at the cardiothoracic surgery ward were admitted from home, 2825 patients (47%, 19 missing) at the cardiology ward, and 5380 patients (71%, 27 missing) at the orthopedics-traumatology ward. The overall percentage of patients discharged to home was 74% at the cardiothoracic surgery ward, 91% at the cardiology ward, and 90% at the orthopedics-traumatology ward. Data were missing from 3 patients at the cardiothoracic surgery ward, 4 patients at the cardiology ward, and 2 patients at the orthopedics-traumatology ward.
Descriptive Characteristics of Patients Admitted to the Cardiothoracic Surgery, Cardiology, and Orthopedics-Traumatology Wardsa
| . | Before . | Implementation . | After . | Total . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| Admissions, n | 912 | 1709 | 1923 | 4544 |
| Age, mean y (SD) | 61.2 (16.4) | 60.9 (16.6) | 61.1 (16.5) | 61.1 (16.6) |
| Males, n (%) | 579 (63%) | 1130 (66%) | 1239 (64%) | 2948 (65%) |
| Surgery, n (%) | 617 (68%) | 1168 (68%) | 1220 (63%) | 3005 (66%) |
| Received PT treatment, n (%) | 583 (64%) | 1207 (71%) | 1289 (67%) | 3079 (68%) |
| No. of PT treatments, mean (SD) | 2.8 (4.7) | 3.4 (5.8) | 3.6 (5.7) | 3.4 (5.6) |
| LOHS, geometric mean (SD) | 4.8 (2.7) | 5.4 (2.7) | 5.1 (2.7) | 5.1 (2.7) |
| Prior living situation, home, n (%) | 522 (57%) | 969 (57%) | 1101 (58%) | 2592 (57%) |
| Discharged home, n (%) | 642 (70%) | 1253 (73%) | 1444 (75%) | 3339 (74%) |
| Cardiology ward | ||||
| Admissions, n | 2489 | 903 | 2646 | 6038 |
| Age, mean y (SD) | 64.7 (15.5) | 65.09 (15.7) | 64.5 (15.7) | 64.7 (15.6) |
| Males, n (%) | 1465 (59%) | 532 (59%) | 1633 (62%) | 3630 (60%) |
| Surgery, n (%) | 76 (3%) | 35 (4%) | 208 (8%) | 319 (5%) |
| Received PT treatment, n (%) | 551 (22%) | 232 (26%) | 752 (28%) | 1534 (25%) |
| No. of PT treatments, mean (SD) | 0.8 (2.5) | 1.2 (4.6) | 1.0 (2.8) | 1.0 (3.0) |
| LOHS, geometric mean (SD) | 2.7 (2.8) | 2.7 (2.8) | 2.6 (2.8) | 2.6 (2.8) |
| Prior living situation, home, n, (%) | 1,110 (45%) | 437 (48%) | 1,278 (49%) | 2,825 (47%) |
| Discharged home, n, (%) | 2,243 (90%) | 807 (89%) | 2,430 (92%) | 5,480 (91%) |
| Orthopedics-traumatology ward | ||||
| Admissions, N | 4332 | 1651 | 1598 | 7581 |
| Age, y [mean (SD)] | 53.2 (18.7) | 53.8 (18.9) | 53.6 (18.7) | 53.4 (18.7) |
| Males, N (%) | 2048 (47%) | 825 (50%) | 818 (51%) | 3691 (49%) |
| Surgery, N (%) | 3627 (84%) | 1357 (82%) | 1315 (82%) | 6299 (83%) |
| Received PT treatment, N (%) | 2340 (54%) | 978 (59%) | 909 (57%) | 4227 (56%) |
| No. of PT treatments, mean (SD) | 2.2 (4.2) | 2.6 (4.3) | 2.8 (4.8) | 2.4 (4.4) |
| LOHS, geometric mean (SD) | 2.1 (3.2) | 2.5 (3.2) | 2.4 (3.4) | 2.3 (3.2) |
| Prior living situation, home, n (%) | 3265 (76%) | 1062 (64%) | 1053 (66%) | 5380 (71%) |
| Discharged home, N (%) | 3934 (91%) | 1462 (89%) | 1452 (91%) | 6848 (90%) |
| . | Before . | Implementation . | After . | Total . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| Admissions, n | 912 | 1709 | 1923 | 4544 |
| Age, mean y (SD) | 61.2 (16.4) | 60.9 (16.6) | 61.1 (16.5) | 61.1 (16.6) |
| Males, n (%) | 579 (63%) | 1130 (66%) | 1239 (64%) | 2948 (65%) |
| Surgery, n (%) | 617 (68%) | 1168 (68%) | 1220 (63%) | 3005 (66%) |
| Received PT treatment, n (%) | 583 (64%) | 1207 (71%) | 1289 (67%) | 3079 (68%) |
| No. of PT treatments, mean (SD) | 2.8 (4.7) | 3.4 (5.8) | 3.6 (5.7) | 3.4 (5.6) |
| LOHS, geometric mean (SD) | 4.8 (2.7) | 5.4 (2.7) | 5.1 (2.7) | 5.1 (2.7) |
| Prior living situation, home, n (%) | 522 (57%) | 969 (57%) | 1101 (58%) | 2592 (57%) |
| Discharged home, n (%) | 642 (70%) | 1253 (73%) | 1444 (75%) | 3339 (74%) |
| Cardiology ward | ||||
| Admissions, n | 2489 | 903 | 2646 | 6038 |
| Age, mean y (SD) | 64.7 (15.5) | 65.09 (15.7) | 64.5 (15.7) | 64.7 (15.6) |
| Males, n (%) | 1465 (59%) | 532 (59%) | 1633 (62%) | 3630 (60%) |
| Surgery, n (%) | 76 (3%) | 35 (4%) | 208 (8%) | 319 (5%) |
| Received PT treatment, n (%) | 551 (22%) | 232 (26%) | 752 (28%) | 1534 (25%) |
| No. of PT treatments, mean (SD) | 0.8 (2.5) | 1.2 (4.6) | 1.0 (2.8) | 1.0 (3.0) |
| LOHS, geometric mean (SD) | 2.7 (2.8) | 2.7 (2.8) | 2.6 (2.8) | 2.6 (2.8) |
| Prior living situation, home, n, (%) | 1,110 (45%) | 437 (48%) | 1,278 (49%) | 2,825 (47%) |
| Discharged home, n, (%) | 2,243 (90%) | 807 (89%) | 2,430 (92%) | 5,480 (91%) |
| Orthopedics-traumatology ward | ||||
| Admissions, N | 4332 | 1651 | 1598 | 7581 |
| Age, y [mean (SD)] | 53.2 (18.7) | 53.8 (18.9) | 53.6 (18.7) | 53.4 (18.7) |
| Males, N (%) | 2048 (47%) | 825 (50%) | 818 (51%) | 3691 (49%) |
| Surgery, N (%) | 3627 (84%) | 1357 (82%) | 1315 (82%) | 6299 (83%) |
| Received PT treatment, N (%) | 2340 (54%) | 978 (59%) | 909 (57%) | 4227 (56%) |
| No. of PT treatments, mean (SD) | 2.2 (4.2) | 2.6 (4.3) | 2.8 (4.8) | 2.4 (4.4) |
| LOHS, geometric mean (SD) | 2.1 (3.2) | 2.5 (3.2) | 2.4 (3.4) | 2.3 (3.2) |
| Prior living situation, home, n (%) | 3265 (76%) | 1062 (64%) | 1053 (66%) | 5380 (71%) |
| Discharged home, N (%) | 3934 (91%) | 1462 (89%) | 1452 (91%) | 6848 (90%) |
aLOHS = length of hospital stay; PT = physical therapy.
Descriptive Characteristics of Patients Admitted to the Cardiothoracic Surgery, Cardiology, and Orthopedics-Traumatology Wardsa
| . | Before . | Implementation . | After . | Total . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| Admissions, n | 912 | 1709 | 1923 | 4544 |
| Age, mean y (SD) | 61.2 (16.4) | 60.9 (16.6) | 61.1 (16.5) | 61.1 (16.6) |
| Males, n (%) | 579 (63%) | 1130 (66%) | 1239 (64%) | 2948 (65%) |
| Surgery, n (%) | 617 (68%) | 1168 (68%) | 1220 (63%) | 3005 (66%) |
| Received PT treatment, n (%) | 583 (64%) | 1207 (71%) | 1289 (67%) | 3079 (68%) |
| No. of PT treatments, mean (SD) | 2.8 (4.7) | 3.4 (5.8) | 3.6 (5.7) | 3.4 (5.6) |
| LOHS, geometric mean (SD) | 4.8 (2.7) | 5.4 (2.7) | 5.1 (2.7) | 5.1 (2.7) |
| Prior living situation, home, n (%) | 522 (57%) | 969 (57%) | 1101 (58%) | 2592 (57%) |
| Discharged home, n (%) | 642 (70%) | 1253 (73%) | 1444 (75%) | 3339 (74%) |
| Cardiology ward | ||||
| Admissions, n | 2489 | 903 | 2646 | 6038 |
| Age, mean y (SD) | 64.7 (15.5) | 65.09 (15.7) | 64.5 (15.7) | 64.7 (15.6) |
| Males, n (%) | 1465 (59%) | 532 (59%) | 1633 (62%) | 3630 (60%) |
| Surgery, n (%) | 76 (3%) | 35 (4%) | 208 (8%) | 319 (5%) |
| Received PT treatment, n (%) | 551 (22%) | 232 (26%) | 752 (28%) | 1534 (25%) |
| No. of PT treatments, mean (SD) | 0.8 (2.5) | 1.2 (4.6) | 1.0 (2.8) | 1.0 (3.0) |
| LOHS, geometric mean (SD) | 2.7 (2.8) | 2.7 (2.8) | 2.6 (2.8) | 2.6 (2.8) |
| Prior living situation, home, n, (%) | 1,110 (45%) | 437 (48%) | 1,278 (49%) | 2,825 (47%) |
| Discharged home, n, (%) | 2,243 (90%) | 807 (89%) | 2,430 (92%) | 5,480 (91%) |
| Orthopedics-traumatology ward | ||||
| Admissions, N | 4332 | 1651 | 1598 | 7581 |
| Age, y [mean (SD)] | 53.2 (18.7) | 53.8 (18.9) | 53.6 (18.7) | 53.4 (18.7) |
| Males, N (%) | 2048 (47%) | 825 (50%) | 818 (51%) | 3691 (49%) |
| Surgery, N (%) | 3627 (84%) | 1357 (82%) | 1315 (82%) | 6299 (83%) |
| Received PT treatment, N (%) | 2340 (54%) | 978 (59%) | 909 (57%) | 4227 (56%) |
| No. of PT treatments, mean (SD) | 2.2 (4.2) | 2.6 (4.3) | 2.8 (4.8) | 2.4 (4.4) |
| LOHS, geometric mean (SD) | 2.1 (3.2) | 2.5 (3.2) | 2.4 (3.4) | 2.3 (3.2) |
| Prior living situation, home, n (%) | 3265 (76%) | 1062 (64%) | 1053 (66%) | 5380 (71%) |
| Discharged home, N (%) | 3934 (91%) | 1462 (89%) | 1452 (91%) | 6848 (90%) |
| . | Before . | Implementation . | After . | Total . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| Admissions, n | 912 | 1709 | 1923 | 4544 |
| Age, mean y (SD) | 61.2 (16.4) | 60.9 (16.6) | 61.1 (16.5) | 61.1 (16.6) |
| Males, n (%) | 579 (63%) | 1130 (66%) | 1239 (64%) | 2948 (65%) |
| Surgery, n (%) | 617 (68%) | 1168 (68%) | 1220 (63%) | 3005 (66%) |
| Received PT treatment, n (%) | 583 (64%) | 1207 (71%) | 1289 (67%) | 3079 (68%) |
| No. of PT treatments, mean (SD) | 2.8 (4.7) | 3.4 (5.8) | 3.6 (5.7) | 3.4 (5.6) |
| LOHS, geometric mean (SD) | 4.8 (2.7) | 5.4 (2.7) | 5.1 (2.7) | 5.1 (2.7) |
| Prior living situation, home, n (%) | 522 (57%) | 969 (57%) | 1101 (58%) | 2592 (57%) |
| Discharged home, n (%) | 642 (70%) | 1253 (73%) | 1444 (75%) | 3339 (74%) |
| Cardiology ward | ||||
| Admissions, n | 2489 | 903 | 2646 | 6038 |
| Age, mean y (SD) | 64.7 (15.5) | 65.09 (15.7) | 64.5 (15.7) | 64.7 (15.6) |
| Males, n (%) | 1465 (59%) | 532 (59%) | 1633 (62%) | 3630 (60%) |
| Surgery, n (%) | 76 (3%) | 35 (4%) | 208 (8%) | 319 (5%) |
| Received PT treatment, n (%) | 551 (22%) | 232 (26%) | 752 (28%) | 1534 (25%) |
| No. of PT treatments, mean (SD) | 0.8 (2.5) | 1.2 (4.6) | 1.0 (2.8) | 1.0 (3.0) |
| LOHS, geometric mean (SD) | 2.7 (2.8) | 2.7 (2.8) | 2.6 (2.8) | 2.6 (2.8) |
| Prior living situation, home, n, (%) | 1,110 (45%) | 437 (48%) | 1,278 (49%) | 2,825 (47%) |
| Discharged home, n, (%) | 2,243 (90%) | 807 (89%) | 2,430 (92%) | 5,480 (91%) |
| Orthopedics-traumatology ward | ||||
| Admissions, N | 4332 | 1651 | 1598 | 7581 |
| Age, y [mean (SD)] | 53.2 (18.7) | 53.8 (18.9) | 53.6 (18.7) | 53.4 (18.7) |
| Males, N (%) | 2048 (47%) | 825 (50%) | 818 (51%) | 3691 (49%) |
| Surgery, N (%) | 3627 (84%) | 1357 (82%) | 1315 (82%) | 6299 (83%) |
| Received PT treatment, N (%) | 2340 (54%) | 978 (59%) | 909 (57%) | 4227 (56%) |
| No. of PT treatments, mean (SD) | 2.2 (4.2) | 2.6 (4.3) | 2.8 (4.8) | 2.4 (4.4) |
| LOHS, geometric mean (SD) | 2.1 (3.2) | 2.5 (3.2) | 2.4 (3.4) | 2.3 (3.2) |
| Prior living situation, home, n (%) | 3265 (76%) | 1062 (64%) | 1053 (66%) | 5380 (71%) |
| Discharged home, N (%) | 3934 (91%) | 1462 (89%) | 1452 (91%) | 6848 (90%) |
aLOHS = length of hospital stay; PT = physical therapy.
All ward-level differences in length of hospital stay and being discharged home are presented per phase in Table 4, adjusted for age, sex, surgery, and physical therapy treatment. At the cardiothoracic surgery ward, there were proportionally more patients discharged home in the implementation phase (OR = 1.21, 95% CI = 1.04 to 1.35) and after implementation (OR = 1.23, 95% CI = 1.07 to 1.37) compared with implementation before. No statistically significant differences were found for the length of hospital stay outcomes. At the cardiology ward, the absolute geometric mean length of hospital stay was 0.22 days lower after implementation (95% CI = −0.29 to −0.14) compared with implementation before. The relative mean length of hospital stay was 11.5% lower after implementation (95% CI = −15.4% to −7.5%) compared with implementation before. Furthermore, there were proportionally more patients discharged home after implementation (OR = 1.37, 95% CI = 1.22 to 1.49) compared with implementation before. No statistically significant differences were found for the length of hospital stay and discharge destination of patients in the implementation phase compared with implementation before. At the orthopedics-traumatology ward, the absolute geometric mean length of hospital stay was 0.32 days higher in the implementation phase (95% CI = 0.11 to 0.55) and 0.28 days higher after implementation (95% CI = 0.06 to 0.50) compared with implementation before. The relative mean length of hospital stay was 8.3% higher in the implementation phase (95% CI = 2.7% to 14.2%) and 7.1% higher after implementation (95% CI = 1.5 to 12.9%) compared with implementation before. No statistically significant differences were found for the discharge destination outcomes.
Differences in LOHS and Patients Discharged Home at Ward Level Between Study Phases, With “Before Implementation” as Referencea
| . | . | Implementation . | After . | P . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| LOHS | Days difference (95% CI) | 0.17 (−0.28 to 0.67) | 0.13 (−0.32 to +0.60) | .76 |
| LOHS | % difference (95% CI) | 2.3% (−3.8% to 9.0%) | 1.7% (−4.3% to 8.1%) | .76 |
| Discharged home | Odds ratio (95% CI) | 1.21 (1.04 to 1.35) | 1.23 (1.07 to 1.37) | .02 |
| Cardiology ward | ||||
| LOHS | Days difference (95% CI) | −0.03 (−0.14 to 0.08) | −0.22 (−0.29 to −0.14) | <.01 |
| LOHS | % difference (95% CI) | −1.8% (−7.6% to 4.4%) | −11.5% (−15.4% to −7.5%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 1.02 (0.72 to 1.25) | 1.37 (1.22–1.49) | <.01 |
| Orthopedics-traumatology ward | ||||
| LOHS | Days difference (95% CI) | 0.32 (0.11 to 0.55) | 0.28 (0.06 to 0.50) | <.01 |
| LOHS | % difference (95% CI) | 8.3% (2.7% to 14.2%) | 7.1% (1.5% to 12.9%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 0.80 (0.54 to 1.01) | 1.09 (0.88 to 1.27) | .06 |
| . | . | Implementation . | After . | P . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| LOHS | Days difference (95% CI) | 0.17 (−0.28 to 0.67) | 0.13 (−0.32 to +0.60) | .76 |
| LOHS | % difference (95% CI) | 2.3% (−3.8% to 9.0%) | 1.7% (−4.3% to 8.1%) | .76 |
| Discharged home | Odds ratio (95% CI) | 1.21 (1.04 to 1.35) | 1.23 (1.07 to 1.37) | .02 |
| Cardiology ward | ||||
| LOHS | Days difference (95% CI) | −0.03 (−0.14 to 0.08) | −0.22 (−0.29 to −0.14) | <.01 |
| LOHS | % difference (95% CI) | −1.8% (−7.6% to 4.4%) | −11.5% (−15.4% to −7.5%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 1.02 (0.72 to 1.25) | 1.37 (1.22–1.49) | <.01 |
| Orthopedics-traumatology ward | ||||
| LOHS | Days difference (95% CI) | 0.32 (0.11 to 0.55) | 0.28 (0.06 to 0.50) | <.01 |
| LOHS | % difference (95% CI) | 8.3% (2.7% to 14.2%) | 7.1% (1.5% to 12.9%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 0.80 (0.54 to 1.01) | 1.09 (0.88 to 1.27) | .06 |
aThe model has been adjusted for mean age, sex, surgery, and physical therapy treatment. An odds ratio >1 indicates proportionally more patients being discharged to home. LOHS = length of hospital stay.
Differences in LOHS and Patients Discharged Home at Ward Level Between Study Phases, With “Before Implementation” as Referencea
| . | . | Implementation . | After . | P . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| LOHS | Days difference (95% CI) | 0.17 (−0.28 to 0.67) | 0.13 (−0.32 to +0.60) | .76 |
| LOHS | % difference (95% CI) | 2.3% (−3.8% to 9.0%) | 1.7% (−4.3% to 8.1%) | .76 |
| Discharged home | Odds ratio (95% CI) | 1.21 (1.04 to 1.35) | 1.23 (1.07 to 1.37) | .02 |
| Cardiology ward | ||||
| LOHS | Days difference (95% CI) | −0.03 (−0.14 to 0.08) | −0.22 (−0.29 to −0.14) | <.01 |
| LOHS | % difference (95% CI) | −1.8% (−7.6% to 4.4%) | −11.5% (−15.4% to −7.5%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 1.02 (0.72 to 1.25) | 1.37 (1.22–1.49) | <.01 |
| Orthopedics-traumatology ward | ||||
| LOHS | Days difference (95% CI) | 0.32 (0.11 to 0.55) | 0.28 (0.06 to 0.50) | <.01 |
| LOHS | % difference (95% CI) | 8.3% (2.7% to 14.2%) | 7.1% (1.5% to 12.9%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 0.80 (0.54 to 1.01) | 1.09 (0.88 to 1.27) | .06 |
| . | . | Implementation . | After . | P . |
|---|---|---|---|---|
| Cardiothoracic surgery ward | ||||
| LOHS | Days difference (95% CI) | 0.17 (−0.28 to 0.67) | 0.13 (−0.32 to +0.60) | .76 |
| LOHS | % difference (95% CI) | 2.3% (−3.8% to 9.0%) | 1.7% (−4.3% to 8.1%) | .76 |
| Discharged home | Odds ratio (95% CI) | 1.21 (1.04 to 1.35) | 1.23 (1.07 to 1.37) | .02 |
| Cardiology ward | ||||
| LOHS | Days difference (95% CI) | −0.03 (−0.14 to 0.08) | −0.22 (−0.29 to −0.14) | <.01 |
| LOHS | % difference (95% CI) | −1.8% (−7.6% to 4.4%) | −11.5% (−15.4% to −7.5%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 1.02 (0.72 to 1.25) | 1.37 (1.22–1.49) | <.01 |
| Orthopedics-traumatology ward | ||||
| LOHS | Days difference (95% CI) | 0.32 (0.11 to 0.55) | 0.28 (0.06 to 0.50) | <.01 |
| LOHS | % difference (95% CI) | 8.3% (2.7% to 14.2%) | 7.1% (1.5% to 12.9%) | <.01 |
| Discharged home | Odds ratio (95% CI) | 0.80 (0.54 to 1.01) | 1.09 (0.88 to 1.27) | .06 |
aThe model has been adjusted for mean age, sex, surgery, and physical therapy treatment. An odds ratio >1 indicates proportionally more patients being discharged to home. LOHS = length of hospital stay.
Sensitivity Analyses
There were no differences between the outcomes of the first sensitivity analysis and the outcomes of the primary analysis. The second sensitivity analysis, to check seasonality, showed 2 outcomes that differed from the primary analysis. The sensitivity analysis indicated no statistically significant higher OR of patients being discharged home in the implementation phase (OR = 1.34, 95% CI = 0.84 to 1.49) and after implementation (OR = 1.20, 95% CI = 0.98 to 1.37) compared with implementation before. In addition, the sensitivity analysis indicated no statistically significantly higher geometric mean length of hospital stay in the implementation phase (mean = +0.09 days, 95% CI = −0.01 to 0.18) and after implementation (mean = +0.03 days, 95% CI = −0.07 to 0.12) compared with implementation before. The third sensitivity analysis, to check the influence of prior living situation, showed 1 outcome that differed from the primary analysis. There were proportionally more patients discharged home (OR = 1.24, 95% CI = 1.06 to 1.39) after implementation at the orthopedics-traumatology ward compared with before implementation.
Discussion
This study is a pragmatic before-after study to evaluate the implementation of an innovative, multifaceted, care intervention to reduce sedentary behavior in adults of all ages during the hospital stay. All implementation activities were performed by the project managers and implementation officers in collaboration with the multidisciplinary care team of the hospital ward. The findings of the ward-level behavioral observations indicate that after implementation of Ban Bedcentricity, patients at the cardiothoracic surgery and cardiology wards are less likely to be in bed during the day. This supports the hypothesis that the implementation of Ban Bedcentricity might reduce sedentary behavior and improve physical activity of patients during the hospital stay. We found statistically significant differences between patients in the “before implementation” and “after implementation” phase, with observations of fewer patients lying in bed (cardiothoracic surgery and cardiology wards), a shorter hospital stay (cardiology ward), and more patients being discharged home (cardiothoracic surgery and cardiology wards). The third sensitivity analysis, including the prior living situation of patients as a covariate in the adjusted model, showed that proportionately more patients were discharged home after implementation at all hospital wards compared with before implementation. Patients after implementation at the orthopedics-traumatology ward had a statistically significantly longer length of hospital stay compared with before implementation.
The findings of this study are not completely unambiguous, especially the differences in outcomes between hospital wards. The first potential rationale for the less promising outcomes at the orthopedics-traumatology ward is the type of complaints for which patients are admitted. A relatively large number of patients are admitted at the orthopedics-traumatology ward with lower extremity fractures. The majority of these patients are not allowed to bear weight on bones and joints in the early phase after surgery because of (restricted) weight-bearing protocols.19 This makes it more difficult to reduce sedentary behavior of patients with the Ban Bedcentricity innovation. Furthermore, the implementation of Ban Bedcentricity at the cardiothoracic surgery and cardiology wards may also have had an impact at the orthopedics-traumatology ward. For example, the managing and medical staff of the different hospital wards meet regularly, and there was hospital-wide attention for the Ban Bedcentricity initiative at several communication platforms. It is possible that the outcomes from the “before implementation” phase at the orthopedic-traumatology ward were influenced by implementation at the other wards so that there was a smaller window for improvement in the implementation phase and after implementation at the orthopedics-traumatology ward.
The outcomes in this manuscript are in line with earlier research showing the benefits of multifaceted interventions for patients aged over 65 years, such as the Mobilisation of Vulnerable Elders in Ontario (MOVE ON) and Hospital Elder Life Program (HELP).20,21 Liu et al20 found less sedentary behavior and a significant shorter length of hospital stay after the pragmatic implementation of MOVE ON. The intervention consisted of a patient-tailored mobility program, supervised by health care professionals, with reminders for patients to mobilize and education for both patients and health care professionals. Strijbos et al22 report lower hospital care costs and lower delirium incidence rates after implementation of HELP, an intervention to maintain physical and cognitive activity of patients during the hospital stay.23,24 Overall, these studies underline the importance of reducing sedentary behavior and improving physical activity in patients during the hospital stay for patients with a variety of ages and diseases. For this purpose, we suggest combining strategies such as an unsupervised, multifaceted intervention tailored to the context of a hospital ward (eg, Ban Bedcentricity) and supervised patient-tailored programs (eg, MOVE ON and HELP).
Strengths and Limitations
This study has several strengths. First, the data on the length of hospital stay and patients being discharged home were routinely and systematically collected in a large sample of 18,163 patients. The dataset contained a few missing values and provided sufficient data for powerful analysis.25 The data analysis was robust with unadjusted, adjusted, and sensitivity analyses showing consistent outcomes. Second, it was both impossible and inappropriate to use individual randomization because the implementation activities focus on individuals, teams, and the hospital environment. The implementation of Ban Bedcentricity has been evaluated in the same way as the use of the implementation activities: pragmatic and tailored to the local hospital context.26 The study design suits the principles of context-based practice, a new concept for research recently introduced in Dutch health care, to improve the interrelation between research and practice.27 The context-based practice approach stimulates the use of explorative, pragmatic research designs with routinely collected data and embraces the relative uncertainty of outcome estimates with the benefits of real-world data.
There are limitations to this study. First, we did not perform a process evaluation of the Ban Bedcentricity implementation procedure. It therefore remains unclear to what extent the different elements of Ban Bedcentricity were perceived, used, and understood (ie, adoption and fidelity) by patients, close relatives, and health care professionals. Our study primarily focused on the evaluation of before-after differences in sedentary behavior, length of hospital stay, and discharge destination at ward level. Less attention was paid to a theoretically sound evaluation of the uptake of the innovation by, for example, examining the knowledge and attitudes of health care professionals or monitoring the use of new materials. Future studies in this domain should consider using the reach, effectiveness, adoption, implementation, and maintenance framework for process evaluation.28 Second, there were no routinely collected data on the physical functioning or prior living situation of patients. Future studies might consider the use of baseline physical function and prior living situation as confounders in their statistical analysis. Third, these outcomes should be interpreted as part of an explorative data analysis in which no causal relationship can be inferred. It is important to emphasize that the findings of this study should be interpreted with caution as a result of common methodological disadvantages such as differences in participant characteristics between study phases.29 By adjusting for mean age, sex, surgery, and physical therapy treatment, the current study aimed to control for (a part of) the differences in participant characteristics.
Implications for Practice
The findings of this study can be used to stimulate the development and evaluation of care interventions across diverse patient contexts. Currently, efficient use of limited health care resources is important in the context of value-based health care.30 The early health technology assessment suggests that a cost-neutral Ban Bedcentricity implementation would be achieved if 15 patients were discharged home 1 day earlier or 1 patient was discharged home instead of to a nursing home per hospital ward per year (Suppl. Mat., files A, B, and C). A cost-effectiveness study might be interesting to estimate the cost-effectiveness of Ban Bedcentricity or similar innovations. Multifaceted interventions to reduce sedentary behavior appear to be examples of value-based health care interventions. However, the effect of our multifaceted innovation on functional decline of patients remains unknown. Future research might focus on the health benefits for patients of, for example, strength, endurance, or functional independence as a result of a multifaceted care intervention implementation. These outcome measures are considered more difficult to collect; however, they are highly clinically relevant.
We have systematically developed, implemented, and evaluated Ban Bedcentricity, a multifaceted innovation to reduce sedentary behavior of patients during the hospital stay by cultural change. Little information is available about the adoption and fidelity of the innovation, and therefore the outcomes should be interpreted with caution. Taking this into account, the current study indicates less sedentary behavior and beneficial differences in ORs of patients being discharged to home after implementation of Ban Bedcentricity compared with implementation before. The outcomes support that Ban Bedcentricity might be an interesting innovation to address the harms associated with prolonged unnecessary bed rest of patients during their hospital stay.
Author Contributions
Concept/idea/research design: N. Koenders, T.J. Hoogeboom
Writing: N. Koenders, S. Potkamp-Kloppers, R. Akkermans, T.J. Hoogeboom
Data collection: N. Koenders, S. Potkamp-Kloppers, Y. Geurts, T.J. Hoogeboom
Data analysis: N. Koenders, S. Potkamp-Kloppers, R. Akkermans, T. J. Hoogeboom
Project management: N. Koenders, Y. Geurts, T. J. Hoogeboom
Fund procurement: Y. Geurts, T. J. Hoogeboom
Providing participants: N. Koenders
Providing facilities/equipment: M.W.G. Nijhuis-van der Sanden, T. J. Hoogeboom
Consultation (including review of manuscript before submitting): S. Potkamp-Kloppers, Y. Geurts, M.W.G. Nijhuis-van der Sanden, T.J. Hoogeboom
Acknowledgments
Hendrikje Rempe and Daphne Maas are acknowledged as important implementation officers. Important advisory officers were, among others, Bertine Lahuis (Board of Directors); Jopie Verhoeven (Patient Advisory Board); Iris Hobo (Department of Construction); and Concha van Rijssel, Lucien Engelen, and Martijn de Groot (REshape Center for Innovation). The authors thank Birgit Jansen and Margot Tacken (Department of Business Intelligence and Analytics) for their independent and anonymous data extraction. Tim Govers and Jan Rongen (Department of Operating Rooms) are thanked for their contributions to the early health technology assessment. The authors thank Frank Klomp for his inspiration and efforts throughout the development of Ban Bedcentricity and Jennifer Cusack for her language corrections to this manuscript. All members of the Dutch expert group Moving Hospitals (in Dutch: Beweegziekenhuizen) are thanked for their help in the study conceptualization.
Funding
This study received an internal innovation grant from Radboudumc University. The study did not receive any additional funding from agencies in the public, commercial, or not-for-profit sector.
Ethics Approval
Ethical approval was granted by the Radboudumc University Ethics Committee (no. 2018–4172), Radboudumc, Nijmegen, the Netherlands.
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
Data Availability
The data that support the findings of this study are available from the corresponding author N.K. upon reasonable request.
References
Robson LS, Shannon HS, Goldenhar LM, Hale AR.
Author notes
Niek Koenders and Sandra Potkamp-Kloppers contributed equally and share first authorship.




Comments